A copay is your share of a medical bill after the insurance provider has contributed its financial portion. Medicare copays (also called copayments) most often come in the form of a flat-fee and typically kick in after a deductible is met.
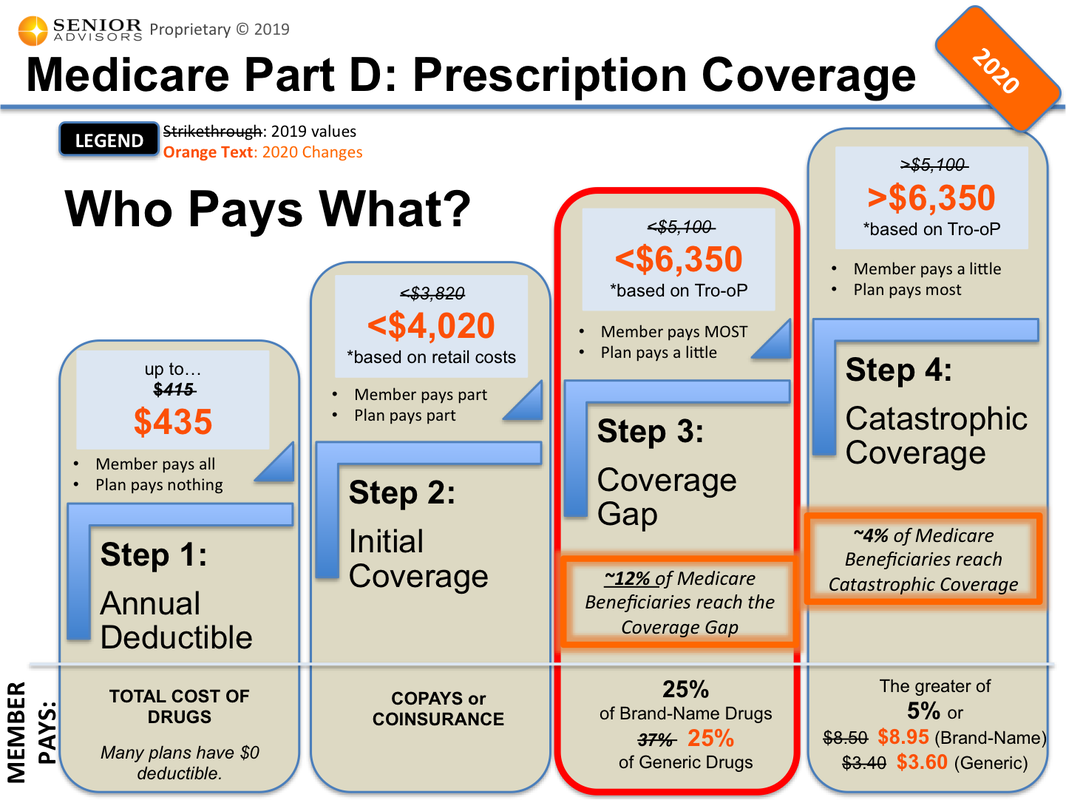
PAPs can provide assistance to Part D enrollees and interface with Part D plans by operating 'outside the Part D benefit' to ensure separateness of Part D benefits and PAP assistance. The PAP's assistance on behalf of the PAP enrollee does not count towards a Part D beneficiary's true-out-of-pocket cost (TrOOP). The calculation of TrOOP is. Deductibles, copayments, coinsurance, tiers, Medicare prescription drug plans, costs, covered prescriptions, generic and brand-name drugs.
Medicare beneficiaries enrolled in the QMB program have no legal obligation to pay Medicare Part A or Part B deductibles, coinsurance, or copays for any Medicare-covered items and services. Despite the federal law, our July 2015 study ('Access to Care Issues Among QMBs') (PDF) found that those in the QMB program were still being wrongly billed. MSPs pay your Medicare Part B premium, and may offer additional assistance. Medicaid can provide cost-sharing assistance: Depending on your income, you may qualify for the Qualified Medicare Beneficiary (QMB) MSP. If you are enrolled in QMB, you do not pay Medicare cost-sharing, which includes deductibles, coinsurances, and copays.
A deductible is the amount you must pay out of pocket before the benefits of the health insurance policy begin to pay.
Understanding Medicare Copayments & Coinsurance
Medicare copayments and coinsurance can be broken down by each part of Original Medicare (Part A and Part B). All costs and figures listed below are for 2021.
Medicare Part A
After meeting a deductible of $1,484, Medicare Part A beneficiaries can expect to pay coinsurance for each day of an inpatient stay in a hospital, mental health facility or skilled nursing facility. Even though it's called coinsurance, it operates like a copay.
- For hospital and mental health facility stays, the first 60 days require no Medicare coinsurance
- Days 61 to 90 require a coinsurance of $371 per day
- Days 91 and beyond come with a $742 per day coinsurance for a total of 60 “lifetime reserve' days
These lifetime reserve days do not reset after the benefit period ends. Once the 60 lifetime reserve days are exhausted, the patient is then responsible for all costs.
For a stay at a skilled nursing facility, the first 20 days do not require a Medicare copay. From day 21 to day 100, a coinsurance of $185.50 is required for each day. Beyond 100 days, the patient is then responsible for all costs.
Under hospice care, you may be required to make copayments of no more than $5 for drugs and other products related to pain relief and symptom control, as well as a 5% coinsurance payment for respite care.
Under Part A of Medicare, a 20% coinsurance may also apply to durable medical equipment utilized for home health care.
Medicare Part B Copays And Deductibles
Medicare Part B
Once the Medicare Part B deductible is met, you may be responsible for 20% of the Medicare-approved amount for most covered services. The Medicare-approved amount is the maximum amount that a doctor or other health care provider can be paid by Medicare.
Some screenings and other preventive services covered by Part B do not require any Medicare copays or coinsurance.
Understanding Medicare Deductibles

Medicare Part A and Medicare Part B each have their own deductibles and their own rules for how they function.
Medicare Part A
The Medicare Part A deductible in 2021 is $1,484 per benefit period. You must meet this deductible before Medicare pays for any Part A services in each benefit period.
Medicare Part A benefit periods are based on how long you've been discharged from the hospital. A benefit period begins the day you are admitted to a hospital or skilled nursing facility for an inpatient stay, and it ends once you have been out of the facility for 60 consecutive days. If you were to be readmitted after 60 days of being home, a new benefit period would start, and you would be responsible for meeting the entire deductible again.
Medicare Part B
The Medicare Part B deductible in 2021 is $203 per year. You must meet this deductible before Medicare pays for any Part B services.
Unlike the Part A deductible, Part B only requires you to pay one deductible per year, no matter how often you see the doctor. After your Part B deductible is met, you typically pay 20 percent of the Medicare-approved amount for most doctor services. This 20 percent is known as your Medicare Part B coinsurance (mentioned in the section above).
Cover your Medicare out-of-pocket costs
There is one way that many Medicare enrollees get help covering their Medicare out-of-pocket costs.
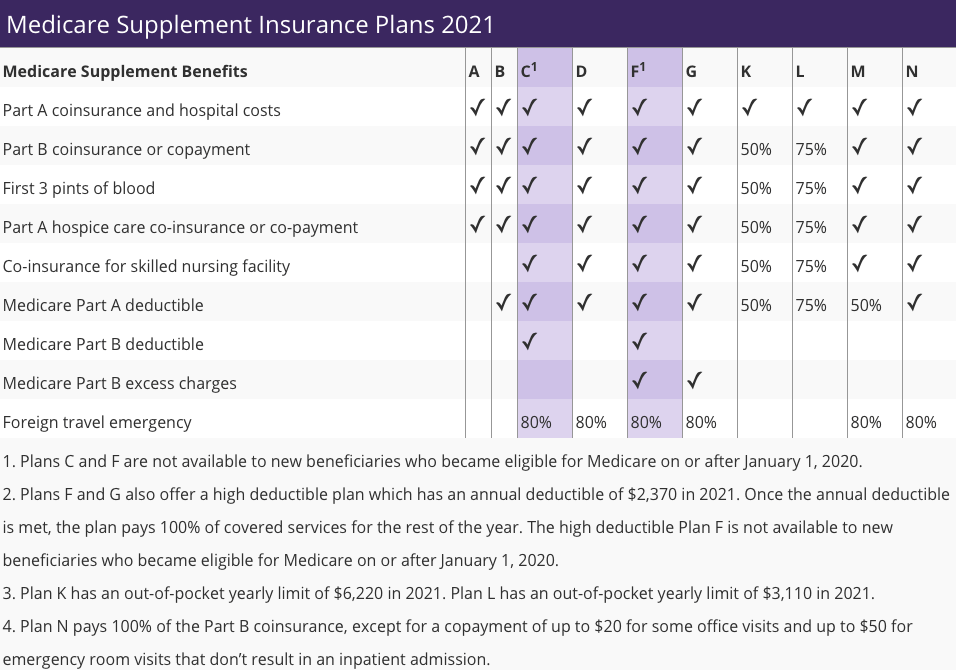
Medigap insurance plans are a form of private health insurance that help supplement your Original Medicare coverage. You pay a premium to a private insurance company for enrollment in a Medigap plan, and the Medigap insurance helps pay for certain Medicare out-of-pocket costs including certain deductibles, copayments and coinsurance.
The chart below shows which Medigap plans cover certain Medicare costs including the ones previously discussed.
Click here to view enlarged chartScroll to the right to continue reading the chart Oxford driver download for windows 10.
Medicare Supplement Benefits
Part A coinsurance and hospital coverage
Part B coinsurance or copayment
Part A hospice care coinsurance or copayment
First 3 pints of blood
Skilled nursing facility coinsurance
Part A deductible
Part B deductible
Part B excess charges
Foreign travel emergency
| A | B | C* | D | F1* | G1 | K2 | L3 | M | N4 |
|---|---|---|---|---|---|---|---|---|---|
| 50% | 75% | ||||||||
| 50% | 75% | ||||||||
| 50% | 75% | ||||||||
| 50% | 75% | ||||||||
| 50% | 75% | 50% | |||||||
| 80% | 80% | 80% | 80% | 80% | 80% |
* Plan F and Plan C are not available to Medicare beneficiaries who became eligible for Medicare on or after January 1, 2020. If you became eligible for Medicare before 2020, you may still be able to enroll in Plan F or Plan C as long as they are available in your area.
+ Read more1 Plans F and G offer high-deductible plans that each have an annual deductible of $2,370 in 2021. Once the annual deductible is met, the plan pays 100% of covered services for the rest of the year. The high-deductible Plan F is not available to new beneficiaries who became eligible for Medicare on or after January 1, 2020.
2 Plan K has an out-of-pocket yearly limit of $6,220 in 2021. After you pay the out-of-pocket yearly limit and yearly Part B deductible, it pays 100% of covered services for the rest of the calendar year.
3 Drivers safa media mobile phones & portable devices. Plan L has an out-of-pocket yearly limit of $3,110 in 2021. After you pay the out-of-pocket yearly limit and yearly Part B deductible, it pays 100% of covered services for the rest of the calendar year.
4 Plan N pays 100% of the Part B coinsurance, except for a copayment of up to $20 for some office visits and up to $50 copayment for emergency room visits that don’t result in an inpatient admission.
- Read lessIf you're ready to get help paying for Medicare out-of-pocket costs, you can apply for a Medigap policy today.
Find Medigap plans in your area.
Find a planResource Center
Enter your email address and get a free guide to Medicare and Medicare Supplement Insurance.
By clicking 'Sign up now' you are agreeing to receive emails from MedicareSupplement.com.
We've been helping people find their perfect Medicare plan for over 10 years.
Ready to find your plan?
There are a number of words and terms related to the way Medicare works, and one of the most important ones to know is coinsurance.
What is Medicare coinsurance?
Coinsurance is the percentage of a medical bill that you (the Medicare beneficiary) may be responsible for paying after reaching your deductible. Coinsurance is a form of cost-sharing; it's a way for the cost of care to be split between you and your provider.
The deductible is the amount you are required to pay in a given year or benefit period before Medicare begins paying its share.
How does Medicare coinsurance work?
Let’s use an example to explain it more clearly.
John has Original Medicare (Part A and Part B) and goes to the doctor for outpatient treatment.
John’s doctor appointment is covered by Medicare Part B, and his doctor bills Medicare for $300. Part B carries an annual deductible of $203 (in 2021), so John is responsible for the first $203 worth of Part B-covered services for the year.
After reaching his Part B deductible, the remaining $97 of his bill is covered in part by Medicare, though John will be required to pay a coinsurance cost.
Medicare Part B requires beneficiaries to pay a 20 percent coinsurance payment after reaching their deductible. This means that John will pay 20 percent of the remaining $97 of his bill, and Medicare Part B will cover 80 percent.
Medicare Part B Copayments
The total amount that John will have to pay for his appointment is $222.40, broken down as follows:
| Total medical bill | $300 |
| 2021 Part B deductible | $203 |
| 20 percent Part B coinsurance of remaining $97 | $19.40 |
| Total beneficiary will pay | $222.40 |
How much is Medicare coinsurance?
Medicare coinsurance is typically 20 percent of the Medicare-approved amount for goods or services covered by Medicare Part B.
So once you have met your Part B deductible for the year, you will then typically be responsible for 20 percent of the remaining cost for covered services and items.
| The Medicare-approved amount is a predetermined amount of money that Medicare has agreed to pay for a covered service or item. |
Private Medicare plans, such as Medicare Advantage and Medicare Part D Prescription Drug Plans (PDP), may feature coinsurance of their own.
While 20 percent is the typical coinsurance amount for Medicare Advantage plans, some plans may feature a 70-30 or 90-10 split.
Medicare Prescription Drug Plans may feature coinsurance or copay amounts that vary depending on the type of drug and what tier that drug is in, according to your Medicare drug plan formulary.
Why does Medicare charge coinsurance?
Cost-sharing measures such as coinsurance (and copays, which you can read more about below) are a way to help keep beneficiaries accountable for their care costs.
With no coinsurance in place, a patient could potentially visit a doctor more frequently for unnecessary health care services after they meet their deductible, because they would pay nothing out-of-pocket for the services.
This would leave the insurance plan carrier to cover all costs of such unnecessary care, which would drive up plan costs for other beneficiaries and contribute to overburdening the health care system.
Cost-sharing is one way of helping ensure that patients are more selective about the type of care they seek.
Coinsurance vs. copays
Copayment, or copay, is another term you’ll see used in relation to Medicare cost-sharing. A copay is like coinsurance, except for one difference: While coinsurance typically involves a percentage of the total medical bill, a copayment is generally a flat fee.
For example, Part B of Medicare uses coinsurance, which is 20 percent in most cases. But Medicare Part A uses copayments for hospital stays, which begin at $371 per day for days 61-90 of an inpatient hospital stay in 2021.
The primary difference between coinsurance vs. copays is that copayments are a flat fee amount instead of a percentage.
Get coverage for Medicare coinsurance
One way you can get some coverage for Medicare coinsurance is by purchasing Medicare Supplement Insurance.
Medicare Supplement Insurance plans (also called Medigap) are optional plans sold by private insurers that offer some coverage for certain out-of-pocket Medicare costs, such as coinsurance, copayments and deductibles.
In exchange for paying a monthly premium to belong to the plan, a Medigap plan can help cover the cost of your Medicare coinsurance and/or your deductibles.
Medicare Part B Doctor Copay
If John from our above example had a Medigap plan that covered his Part B deductible and coinsurance, he may have owed nothing for his doctor’s appointment.
Medicare Advantage plans typically include coinsurance
Many Medicare beneficiaries choose to get their benefits through a privately-sold Medicare Advantage plan (Medicare Part C), which provides the benefits of Original Medicare combined into one plan.
Many Medicare Advantage plans may also offer prescription drug coverage, as well as coverage for hearing, dental and vision care, which are not typically covered by Original Medicare.
While a Medicare Advantage plan will likely include coinsurance costs, a plan could help you save on some of your other out-of-pocket health care costs, which could help offset some of your coinsurance payments.
To learn more about Medicare Advantage and to compare the plan options available in your area, call to speak with a licensed insurance agent today.
Medicare Part B Copay Assistance
Explore Medicare Advantage plan benefits in your area
Medicare B Guidelines Physical Therapy
Or call 1-800-557-60591-800-557-6059TTY Users: 711 to speak with a licensed insurance agent. We accept calls 24/7!

Comments are closed.